Les adhésifs résistants à l'autoclave peuvent être la solution
La chaleur, l'humidité, les produits chimiques et d'autres facteurs environnementaux peuvent poser des problèmes aux outils médicaux tels que les endoscopes, les instruments chirurgicaux, les équipements dentaires, les dispositifs médicaux à usage général et les assemblages de boîtiers, ainsi qu'aux capteurs et aux étiquettes RFID collés aux outils médicaux. Les matériaux qui lient, recouvrent et encapsulent les composants de ces dispositifs peuvent être affectés négativement par ces forces, ce qui peut potentiellement entraîner une défaillance de l'appareil, la perte ou l'égarement des instruments ou des blessures au patient. C'est pourquoi il est essentiel que les produits utilisés pour protéger et lier les pièces entre elles soient capables de tolérer une variété de contraintes.
Outre les types rigoureux de tests physiques, de normes et d’approbations qui formulations de dispositifs médicaux sont soumis à des normes telles que la norme ISO 10993 ; beaucoup doivent également pouvoir résister à des cycles répétés de stérilisation.
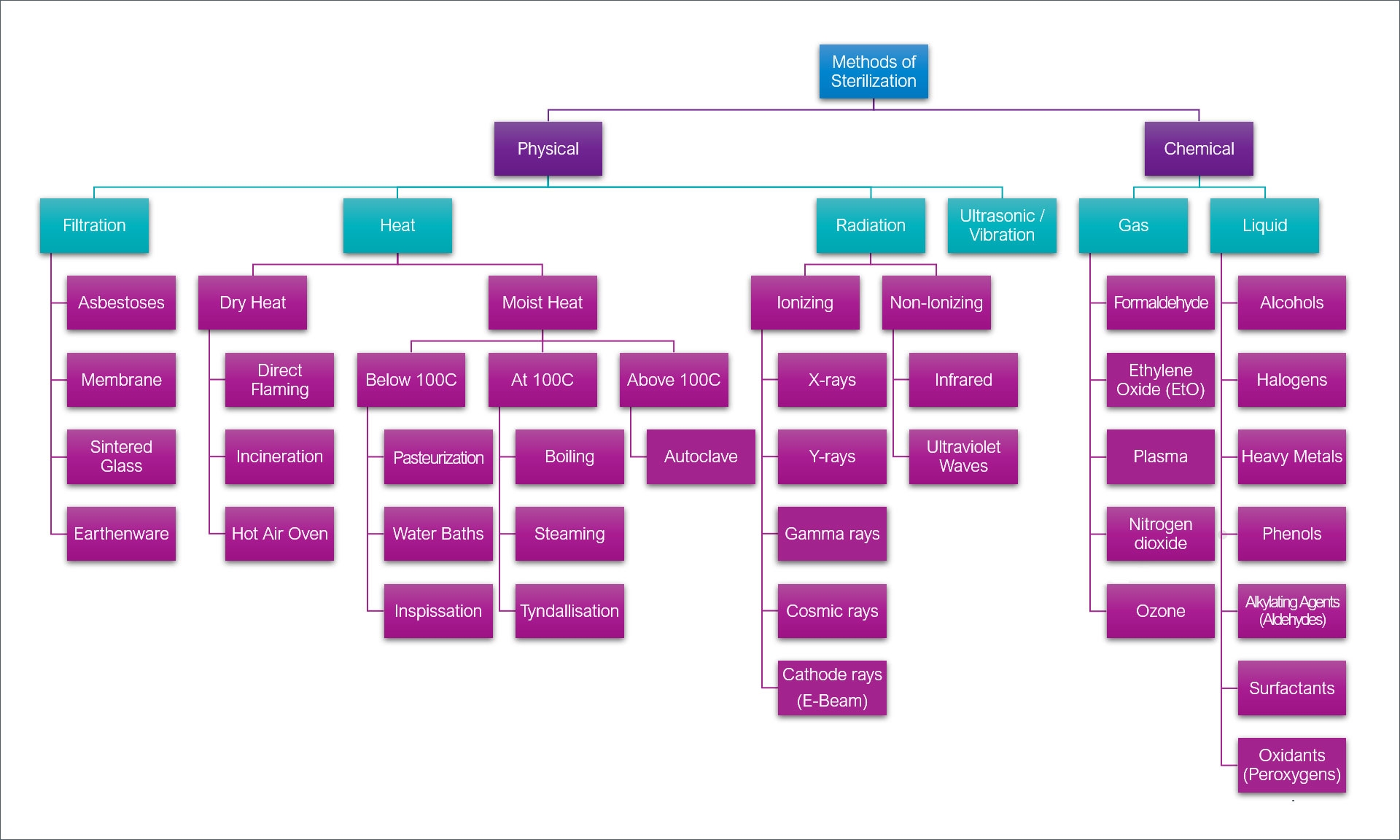
Deux catégories de stérilisation utilisées dans l'industrie des dispositifs médicaux sont classées comme physiques ou chimiques. Les méthodes de stérilisation physique comprennent la filtration, la chaleur, les radiations et les ultrasons/vibrations, tandis que la stérilisation chimique nécessite un procédé gazeux ou liquide. Il existe un large sous-ensemble de techniques qui relèvent de ces classes principales, telles que l'EtO, les rayons gamma, les faisceaux d'électrons, les rayons cathodiques et les oxydants, ainsi que l'autoclave et le peroxyde d'hydrogène-plasma STERRAD™.
Les types de méthodes de stérilisation physiques et chimiques couramment utilisées dans l’industrie médicale.
L'utilisation de ces procédés présente des avantages et des inconvénients. Les avantages et les résultats positifs, selon la méthode choisie, comprennent une capacité de pénétration élevée, une action très rapide contre les micro-organismes et l'élimination des résidus potentiels. Certains des facteurs négatifs peuvent inclure des cycles de stérilisation longs, l'inflammabilité, l'utilisation de matières ou de produits chimiques dangereux, le jaunissement des polymères et la corrosion de divers substrats métalliques.
Le choix du type de stérilisation à utiliser dépend du produit final, de sa fonction, des composants du substrat et des pressions et environnements auxquels le dispositif sera soumis. L'autoclave (vapeur) et le plasma au peroxyde d'hydrogène (HPGP) sont deux méthodes souvent utilisées dans l'industrie des dispositifs médicaux.
L'autoclavage utilise de la vapeur sous haute pression pour stériliser les instruments et les débarrasser des micro-organismes et des bactéries susceptibles de contaminer les surfaces des substrats en les tuant et en les rendant inefficaces. Cependant, il faut garder à l'esprit certains problèmes critiques. De nombreux métaux peuvent se corroder ou rouiller après une exposition répétée à la vapeur. Certains plastiques peuvent perdre leur intégrité structurelle, être sensibles à des niveaux de chaleur élevés, être susceptibles de voir migrer des plastifiants vers la surface du substrat ou réagir négativement ou se décomposer lorsqu'ils sont exposés à l'eau.
La stérilisation par autoclavage est limitée à certaines applications. De nombreux adhésifs pour dispositifs médicaux, par exemple, ont du mal à résister à l'autoclavage en raison de la température, de l'humidité et de la pression élevées impliquées dans le processus. En raison de ces facteurs, il peut y avoir un joint de liaison affaibli qui se rompt. Des alternatives à la stérilisation à la vapeur pour les instruments et dispositifs sensibles à la chaleur et à l'humidité sont envisagées de plus en plus régulièrement, bien que l'autoclave reste l'une des options les plus accessibles pour les hôpitaux, les laboratoires, les centres de recherche, etc.
La stérilisation STERRAD™ est une méthode idéale pour les appareils sensibles à la chaleur et à l'humidité, car les températures ne dépassent pas environ 56 °C (133 °F) pendant le traitement. Une solution de peroxyde d'hydrogène et d'eau est délivrée au stérilisateur, puis vaporisée dans la chambre. La solution entoure et interagit avec les appareils et crée un environnement biocide qui inactive les micro-organismes. Un champ électrique puissant est appliqué à la chambre et crée un plasma gazeux de peroxyde d'hydrogène qui dissocie les molécules de peroxyde d'hydrogène en espèces énergisées. Une fois le champ électrique désactivé, les espèces énergisées se recombinent, ce qui transforme le peroxyde d'hydrogène en eau et en oxygène. Cela garantit que les instruments sont rapidement stérilisés sans aucun résidu toxique.
De nombreux types d'endoscopes et d'appareils médicaux nécessitent des cycles de stérilisation répétés ou plusieurs cycles d'autoclavage ou des méthodes de stérilisation alternatives comme la stérilisation au peroxyde d'hydrogène et au plasma.
Liste d'échantillons de lunettes nécessitant plusieurs cycles de stérilisation
Arthroscopes
Bronchoscopes
Les coloscopes
Duodénoscopes
Endoscopes
Oesophagoscopes
Instruments laparoscopiques
Exemple de liste d'appareils supplémentaires
Outils/équipements dentaires
Outils/équipements ophtalmiques
Outils/instruments chirurgicaux
Accessoires pour biopsie endoscopique (généralement des outils, par exemple des pinces)
Systèmes d'irrigation (ex. canules d'irrigation réutilisables)
L'une des applications importantes qui est devenue une priorité dans le secteur des dispositifs médicaux est l'utilisation d'étiquettes d'identification, ou RFID (identification par radiofréquence), sur les outils chirurgicaux, les instruments et les emballages tels que les flacons. Les RFID sur les instruments médicaux aident à maintenir des niveaux de stock précis et à en assurer le suivi pendant les procédures. D'autres domaines d'utilisation et applications typiques comprennent :
Hôpitaux, cliniques et soignants :
- « Check in / check out » la multitude d’appareils et d’outils nécessaires aux interventions et aux chirurgies
− En raison de cas d’outils ou d’accessoires laissés dans le corps après une intervention chirurgicale - Valider l'état de stérilisation avant utilisation
- Améliorer les détails et les données de l'inventaire
Autres domaines de la santé :
- Suivi pharmaceutique pour garantir que le dosage approprié est fourni et que les conditions de stockage appropriées sont respectées
- Suivi des échantillons sanguins/biologiques pour le stockage, les temps d'utilisation et le suivi automatique pour garantir une manipulation appropriée
- Des actifs tels que des outils chirurgicaux, du matériel dentaire et hospitalier, des patients et autres
Les RFID qui sont apposées sur les outils chirurgicaux fréquemment utilisés et sur les matériaux utilisés pour les coller doivent passer plusieurs étapes de stérilisation et réussir à supporter ces processus pendant des centaines de cycles.
Application d'un agent d'encapsulation appliqué sur une puce RFID fixée à une pince médicale.
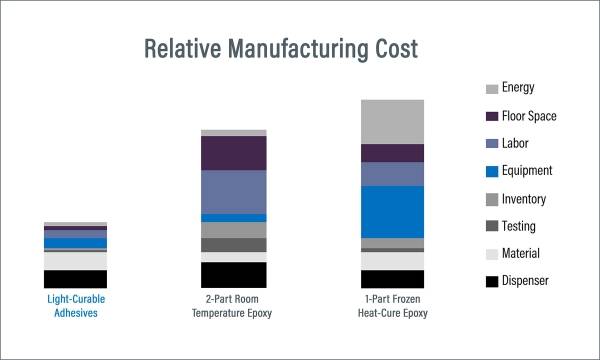
Bien qu'il existe sur le marché des époxydes formulés en une ou deux parties pour le collage, le revêtement et encapsulation dispositifs médicaux et RFID, Ces produits ne constituent peut-être pas le meilleur choix. Par rapport aux matériaux photopolymérisables, les époxydes présentent de nombreux inconvénients, tels que des systèmes de mélange spécialisés, des temps de polymérisation longs pouvant atteindre 60 minutes, une durée de vie en pot courte, l'utilisation de fours de durcissement thermique (dans certains cas), une flexibilité et une résistance aux chocs inférieures, et la nécessité de cycles de purge pouvant entraîner des déchets dangereux. Les adhésifs polymérisables monocomposants offrent une alternative à ces solutions en offrant aux fabricants des temps de polymérisation rapides de 1 à 30 secondes, aucun mélange ni purge, une gamme de qualités allant du rigide au flexible, des formulations conformes à la directive RoHS et sans ajout de solvants pour une manipulation et une élimination plus faciles. Les avantages positifs des matériaux photopolymérisables peuvent contribuer à améliorer l'efficacité de la fabrication, à réduire les coûts et à augmenter le rendement.
Pour répondre au besoin d'un produit capable de survivre à des séquences de stérilisation fréquentes, une nouvelle solution polyvalente Adhésif polymérisable par UV/LED a été développé pour présenter une absorption d'eau extrêmement faible (0,5 %) et résister à plus de 100 cycles de processus en autoclave et au plasma. Ce matériau est recommandé pour une utilisation comme revêtement ou agent d'encapsulation pour les assemblages de boîtiers, les instruments médicaux à usage unique ou multiple, ainsi que pour une variété d'instruments médicaux et d'équipements dentaires. Il est particulièrement adapté à encapsulation de puces RFID, de capteurs et d'autres composants électroniques présents sur les dispositifs médicaux, les outils et les flacons où l'infiltration d'humidité peut être préoccupante. Les substrats collables comprennent l'acier inoxydable, l'aluminium, le verre, le PP/PE et les circuits imprimés.
L'adhésif a été soumis à une série de tests de performance comprenant le vieillissement accéléré et la stérilisation, l'évaluation de l'imprégnation dans l'eau, l'examen des propriétés électriques et le test du taux de transmission de la vapeur d'eau. Conforme aux normes de cytotoxicité ISO 10993-5, le matériau durcit en quelques secondes après exposition à une lumière UV à large spectre ou à une lumière LED 365 nm.
Si vous êtes un fabricant impliqué dans l'assemblage et la protection de dispositifs et d'instruments médicaux et que vous recherchez un matériau de collage, de revêtement et encapsulation capable de résister à plus de 100 cycles de stérilisation, ce produit peut être une solution pour votre application.
STERRAD™ est une marque déposée d'ASP Global Manufacturing, GmbH.